[:en]Wim J.A. van den Heuvel, PhD, Honorary Professor, University of Groningen, the Netherlands.
Address for correspondence: heuvelwim@hotmail.com
Abstract
Objective:
This paper analyses which countries in Europe did increase or decrease their end-of-life care efforts in the last five years. It describes the overall ranking of 27 European countries on the 2015 Quality of Death Index and it compares the changes in ranking on the Quality of Death Index of 22 European countries between 2010 and 2015.
Method:
To assess changes in quality of palliative care the scores and ranking of the Quality of Death Index of 2010 and 2015 were compared. The comparison was made on the Quality of Death Index as well as on two of its domains: affordability of palliative care and quality of care.
Results:
The countries ranking highest on the Quality of Death Index are situated in West-North Europe, the lowest ranking ones in East-South Europe. There is a wide gap between countries ranking high and low. Efforts to improve palliative care vary over time within countries. In Austria and Hungary the ranking on the quality of death index decreased, but in Finland and Portugal the index increased significantly. Overall, the comparison of ranking shows that ´negative´ changes in ranking between 2010 and 2015 seem more frequently in Central/-Eastern European countries as compared to Scandinavian and Southern-West European countries.
Conclusion:
The comparison of ‘quality of death’ between 22 European countries indicates that palliative care lacks to be an integral part of health care. This applies especially to Central-Eastern European countries. In half of the participating European countries the quality of death did not improve over the last five years. Almost half of the European countries provide insufficient palliative care services for their suffering citizens.
Key words: palliative care, end-of-life care, quality of death, international comparison
Introduction
In 2010 the Economic Intelligence Unit (EIU) published a study on `Quality of Death´ of 40 countries, including 24 European ones (1). Based on 4 domains (with 24 indicators) a ´Quality of Death Index´ was composed. The index intended to assess the quality of end-of-life care in each country (1).
Assessment of quality of palliative care per country is important because it may show what efforts governments make to reduce suffering of citizens, i.e. patients with long-term care needs and/or terminal diseases, and how these governments concern about the quality of life for those patients as well as for their beloved ones. Assessment of quality of end-of-life care is also relevant because recent studies indicate that adequate palliative care may safe health care costs, which costs are a major concern for many governments, especially in ageing societies (2).
A comparison between countries on the quality of their end-of-life care may contribute to improve palliative care services nationwide and internationally. Comparative studies also demonstrate the cultural differences between countries in the awareness and acceptance of death and dying (3, 4).
Recently the EIU published the 2015 ´Quality of Death Index´ (5). In this study the number of countries as well as the number of domains are extended. Although therefore direct comparisons between the scores of 2010 and 2015 are not possible, the report concludes that ´some countries are stepping up their effort to ensure all citizens have access to palliative care´ (5).
The question in this paper is which countries in Europe did step up or not, i.e. which European countries did increase or decrease their quality of end-of-life care efforts based on the ranking on the Quality of Death Index? The choice for Europe is based on the large number of European countries which are included in both studies of the EIU.
This paper will describe the overall ranking of the 27 European countries which participated in the 2015 Quality of Death Index. Next a comparison will be made between the 22 European countries who participated in the studies of 2010 and 2015.
Methods
As stated the method to assess the Quality of Death Index differs between the one of 2010 as compared to the one of 2015.
The four domains used in the 2010 to construct the ´Quality of Death Index´ were: basic end-of-life healthcare environment (10 indicators), availability of end-of-life care (4 indicators), costs of end-of-life care (3 indicators), and quality of end-of-life care (7 indicators) (1). The scores of the European countries in the 2010 Quality of Death Index are scaled from 0 to 10.
In 2015 five domains with in total 20 indicators were used: palliative and health care environment (4 indicators), human resources (5 indicators), affordability of care (3 indicators), quality of care (6 indicators), and community engagement (2 indicators) (5). The overall ranking of the European countries involved in the 2015 Quality of Death Index is based on the total score of the index, which may vary from 0 to 100.
For a comparison between the participating European countries in 2010 and 2015 the ranking will be used because the way the actual scores are calculated differs between 2010 and 2015. The following variables will be used for comparison: the Quality of Death Index, the domain affordability of palliative care, and the domain quality of care.
As is stated in the 2015 report, the Quality of Death Index of 2010 and 2015 may be used for comparison, although they differ in the way they are composed (5). The domain affordability of palliative care of 2015 was called ‘costs of end-of-life care’ in 2010, but the same 3 indicators were used. The domains quality of end-of-life care (in 2010) and quality of care (in 2015) share 4 indicators.
The total number of European countries of which these data over both years are available is 22. For comparison the changes in ranking between 2010 and 2015 are an indication for an increase or decrease of efforts in palliative care per country. Also it may show which countries made more effort than others.
Results
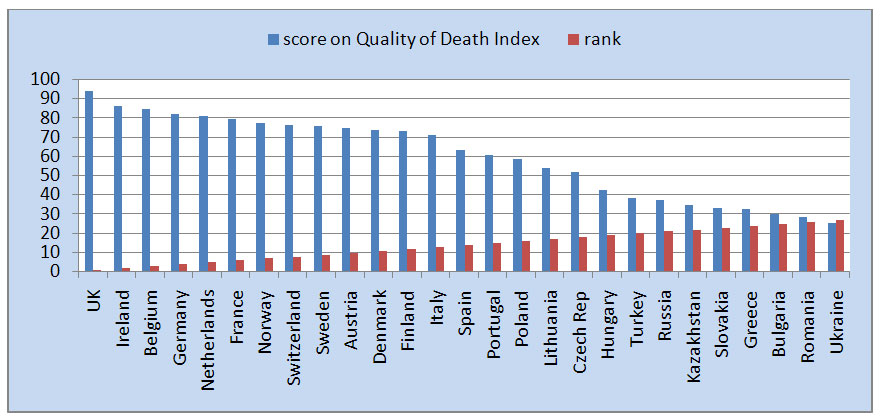
The scores on the quality of death index in the 27 participating European countries varies from 93.9 for the UK (rank 1) to 25.5 for the Ukraine (rank 27) (see figure 1). It is a wide gap in scores within Europe. It indicates it is better to die in the UK than in the Ukraine. The countries ranking highest on the Quality of Death Index are situated in West-North Europe, the lowest ranking ones in East-South Europe.
Figure 1- Scores on Quality of Death Index in participating European countries 2015 (source 5)
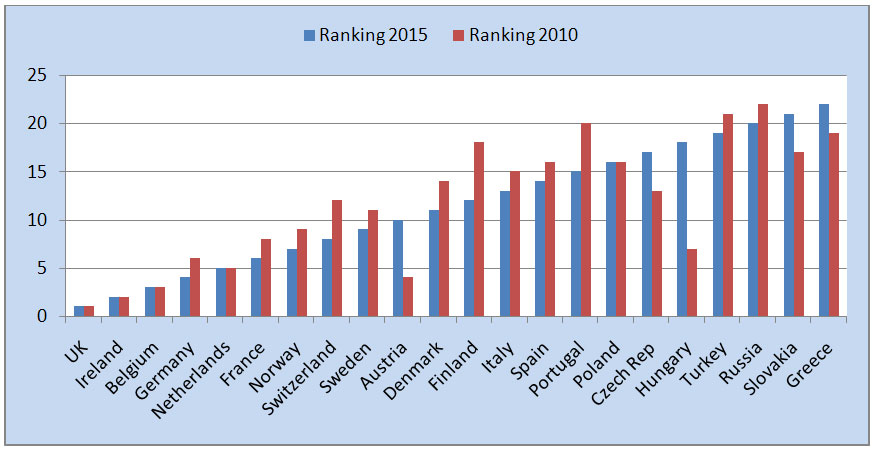
However, the level of quality of death index varies over time. The differences in ranking between the assessments of 2010 and 2015 indicate which states did increased their efforts to improve the quality of death in five years and which did not. The comparison shows that in Austria and Hungary the ranking on the quality of death index evidently decreased, but in Finland and Portugal increased (see figure 2). Austria being on rank 4 in 2010 was on rank 10 in 2015 and Hungary was on rank 7 in 2010 and on rank 18 in 2015.
Figure 2 – Ranking on Quality of Death Index in between 2015 and 2010 of 22 European countries
(sources 1 and 5)
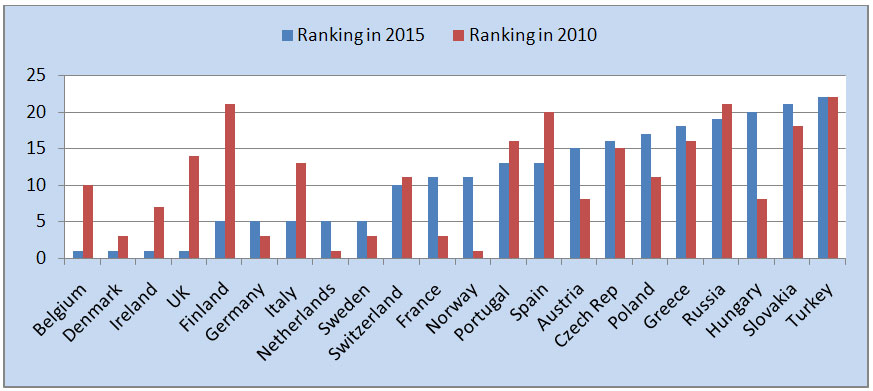
The ranking of Finland, the UK, Belgium, Italy, Ireland, Spain, and Portugal on the domain ´affordability of palliative care´ improved strongly between 2010 and 2015, indicating that more public funding was available for patients in need for palliative care in 2015 as compared to 2010 and that criteria and procedures to receive such care were improved (see figure 3). The reverse seems the case in Norway, Hungary, France, and Austria.
Figure 3 – Ranking on affordability of palliative care of 22 European countries in 2015 and 2010 (sources 1, 5)
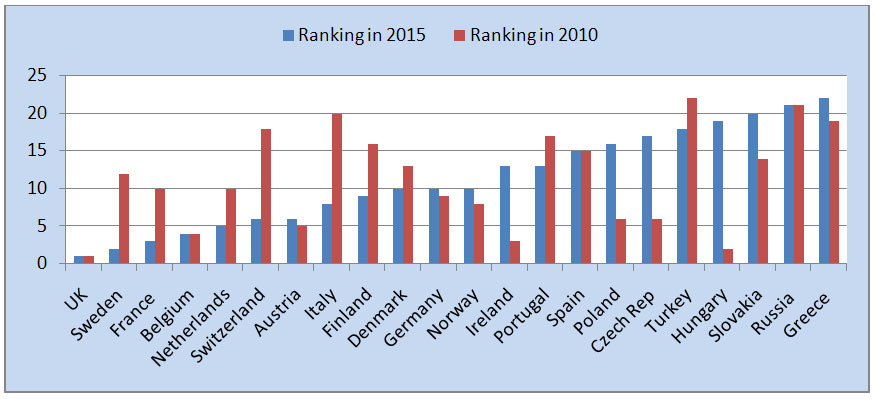
In the domain of ´quality of palliative care´ (including indicators as presence of accreditation and standards for palliative care, availability of opioid painkillers, presence of do-not-resuscitate policy, and shared decision making) the ranking in Italy, Sweden, Finland, Switzerland, and France strongly improved, while the ranking in Hungary, Czech Republic, Poland, Ireland, and Slovakia evidently decreased (see figure 4).
Figure 4 – Ranking on quality of care of 22 European countries in 2015 and 2010 (sources 1, 5)
Overall, the comparison shows that ´negative´ changes in ranking between 2010 and 2015 seem more frequently in Central/-Eastern European countries as compared to Scandinavian and Southern-West European countries. The comparison also shows that the ranking of some countries increases on one domain but decreases on another. For example, France ‘looses’ 7 ranks in the affordability domain, but ‘wins’ 7 in the quality domain. A more detailed overview of the European countries, who changed 5 or more positions on ranking (positive or negative) between 2010 and 2015 shows that the ranking on the 2 domains (affordability of palliative care and quality of care) increased strongly in Finland and Italy, but decreased strongly in Hungary and Poland (see Overview 1).
Overview 1 – Changes in five ranking positions or more on the Quality of Death Index, affordability of palliative care, and quality of care between 2010-2015 (sources 1, 5)

Discussion
The 2015 Quality of Death Index presents a worldwide picture on the way governments try to realise the availability and quality of palliative care. In this paper the situation in Europe is described. The worldwide picture of the Quality of Death Index is not positive. As was concluded by WHO, worldwide 86% of people in need for palliative care do not receive it (6). The situation in Europe is as compared to the 80 countries worldwide rather positive. However, within Europe some countries rank low also when compared with the worldwide situation. Of the 80 countries worldwide, Ukraine is ranked on place 69, Romania on 64, and Bulgaria on 62. Of we consider a score of 50 or higher on the 2015 Quality of Death Index as ‘sufficient’, also Greece, Slovakia, Kazakhstan, Russia, Turkey, and Hungary score ‘insufficient’. Insufficient scores in Europe concentrate in Eastern Europe.
Comparison between the 2015 and 2010 Quality of Death Index opens the opportunity to compare whether ´some countries are stepping up their effort to ensure all citizens have access to palliative care´ as the 2015 report states (5). While comparison of scores is not possible, the interpretation of differences in ranking is not easy. Nevertheless, our analysis indicates that some countries have made real progress (for example Finland and Italy) in improving conditions for palliative care, while investments in improving palliative care of other countries (for example Hungary, Austria and Poland) may be questioned.
It seems that former investments in palliative care in Central-Eastern European countries are not continued. An explanation may be that initiatives to stimulate palliative care in Central-Eastern European countries in the beginning of this century was taken by charity funds and non-profit institutions from abroad, while commitment of national ministries and policy makers was not ensured. In the EIU reports Romania is used as an example. In 2010 Romania was qualified as a beacon for the development of palliative care: ‘from last to leader’, thanks to funding by UK charity funds. In 2015 the situation in Romania is deteriorated. The 2015 report states that ‘to cope with future demand, countries need to embrace the public health model of palliative care and to extend palliative care into a broad range of health care services’(5; p 37). This is evidently not the case in Romania or in Hungary.
The comparison of ‘quality of death’ between 22 European countries underlines the WHO resolution that palliative care need to be an integral part of health care (7). This applies especially to Central-Eastern European countries. This means policy makers in these countries should take responsibility for the availability and quality of palliative care (i.e. funding and standards). Also, health care professionals should be trained in end-of-life care and the public awareness on death and dying needs to be stimulated. The ‘2015 Quality of Death Index’ report recommends a needed change in the culture of health care: ‘moving from a culture of curing illness to managing long-term conditions’ (5).
The answer on the question of this paper is: palliative care did not improve in Europe during the last 5 years. Palliative care improved in a few countries. Palliative care has a stable, high quality position in about 5-6 European countries, but even ´top/ranked nations currently struggle to provide adequate palliative care services for every citizen´ (5; p 6). About half of the European countries provide insufficient palliative care services for their suffering citizens.
References
1. The Quality of Death Index. Ranking end-of-life care across the world. Economic Intelligence Unit. Hong Kong.2010.
2. Smith S, Brick A, O´Hara S, Normand C. Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat Med 2014; 28 (2):130-150.
3. Coolen PR. Cultural Relevance in End-of-Life Care. [Available at: http://ethnomed.org/clinical/end-of-life/cultural-relevance-in-end-of-life-care.
4. Lobar SL, Youngblut JM, Brooten D. Cross-cultural beliefs, ceremonies, and rituals surrounding death of a loved one. Pediatr Nurs 2006;32(1):44-50.
5. The 2015 Quality of Death Index. Ranking palliative care across the world. Economic Intelligence Unit Limited. Hong Kong.2015.
6. World Health Organisation 2015 Palliative care. Fact sheet Nr 402 http://www.who.int/mediacentre/factsheets/fs402/en/
7. Strengthening of palliative care as a component of integrated treatment within the continuum of care. http://apps.who.int/gb/ebwha/pdf_files/EB134/B134_R7-en.pdf
Conflict of interest: none
Received: 18 September 2015
Accepted: 1 October 2015[:ro]Wim J.A. van den Heuvel, PhD, profesor onorific, Universitatea din Groningen, Olanda
Adresa pentru corespondență: heuvelwim@hotmail.com
Rezumat
Obiective:
Această lucrare își propune să analizeze care dintre țările din Europa au înregistrat în ultimii cinci ani o creștere sau descrește a calității îngrijirii acordată la sfârșitul vieții. Se descrie clasamentul după Indicele de Calitate a Morții din 27 de țări europene în 2015 și se compară schimbările survenite în acest clasament în 22 de țări europene, între 2010 și 2015.
Metodă:
Pentru a evalua calitatea îngrijirilor paliative au fost comparate scorurile și clasamentul după Indicele de Calitate a Morții între 2010 și 2015. Pe lângă scorurile globale și clasificarea după Indicele de Calitate a Morții, comparația a fost făcută pe alte două domenii ale acestui indice: accesibilitate la îngrijiri paliative și calitatea îngrijirii acordată la sfârșitul vieții.
Rezultate:
Țările din clasament cu cel mai ridicat Indicelui de Calitate a Morții se află în Europa de Vest și de Nord, iar cele cu cel mai scazut indice, în cele din Europa de Est și de Sud. Există un decalaj destul de mare între țări și între cel mai înalt și cel mai scăzut loc din clasament. Eforturile de a dezvolta îngrijirea paliativă variază în timp în interiorul țărilor. În Austria și Ungaria calitatea acestui indice a scăzut, dar în Finlanda și Portugalia ea a crescut. În general, schimbările ‘negative’ în clasament între 2010 și 2015 par a fi mai frecvente în Europa Centrală și de Est în comparație cu țările scandinave și europene din vest și din sud.
Concluzii:
Compararea Indicelui de Calitate a Morții între 22 de țări europene indică faptul că îngrijirea paliativă trebuie să fie o parte integrantă a asistenței medicale. Acest lucru este valabil în special pentru țările din Europa Centrală și de Est. În jumătate dintre țările participante Indicele de Calitate a Morții nu s-a îmbunătățit în ultimii cinci ani. De asemenea, aproape jumătate din țările europene oferă servicii de îngrijire paliativă insuficiente pentru cetățenii lor aflați în suferință.
Cuvinte cheie: îngrijiri paliative, îngrijirea acordată la sfârșitul vieții, calitatea morții, comparație la nivel international
[:]

One Comment